Weight in Kilograms: Intervention Bundle
The National Pediatric Readiness Project (NPRP) is a multi-phase, multidisciplinary, longitudinal quality initiative to improve the readiness of United States (U.S.) emergency departments (EDs) to care for children. It is supported by the Health Resources and Services Administration, Maternal and Child Health Bureau, Emergency Medical Services (EMS) for Children Program and is co-sponsored by the American Academy of Pediatrics (AAP), the American College of Emergency Physicians (ACEP), and the Emergency Nurses Association (ENA). This initiative has grown significantly over the last two decades and has included two web-based national assessments of pediatric readiness based on published national guidelines.(1-5) The first was completed in 2013 and 83 percent of EDs across the US participated which was a clear indication of the nation’s desire to ensure high-quality emergency care for children.(6) The second was completed in August 2021 and 3642 emergency department leaders responded representing 71% of EDs across the nation.(7) Subsequent research has shown an important association of pediatric readiness, as measured in these national assessments, with the outcome of care of children.(8-10) More specifically, highly pediatric-ready EDs are associated with reduced mortality rates for children with critical illness and injury. Gaps that are immediately actionable and that can improve pediatric readiness and enhance patient safety include the following:
- Presence of physician and nurse pediatric emergency care coordinators (PECC)
- Presence of quality improvement plans that include children
- Staffing the ED with board-certified emergency physicians
- A process to ensure pediatric weights are measured in kilograms
This intervention bundle focuses on the weighing of children in metric units. Over the past 15 years, patient safety has become a key priority for health systems.(11) The American Academy of Pediatrics published many statements addressing pediatric patient-specific safety issues.(12,13) In pediatric patients, many factors contribute to the risk of medication errors, including weight-based dosing, off-label drug use, decreased communication abilities, an inability to self-administer medications, and the high vulnerability to harm of young, critically ill, and injured children, particularly those with immature renal and hepatic systems.(14)
This intervention bundle is designed to help guide PRQC teams that want to implement change strategies specific to the clinical care process for children who present to the ED and require weight-based dosing. Teams can select to work on an intervention specific to weighing children in kilograms for their quality improvement project.
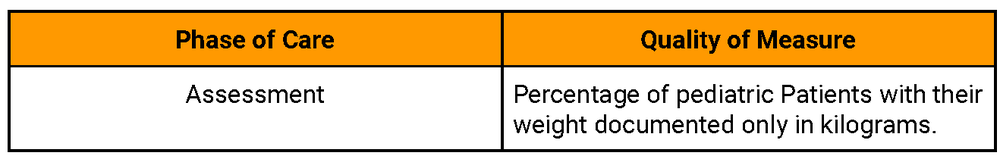
It is anticipated that individual hospital/facility teams will choose one or more measures to work on. The following measures are included within the National Pediatric Readiness Quality Initiative (NPRQI), where you will enter select data. Please see here to learn more about quality measures development.
The quality measures related to weighing children in kilograms are:
Gathering data when implementing change to your system is important to both track how your implementation is going and also to assess whether your changes are moving towards your process measure goal. Data can help give insight into how the changes are being accepted or not accepted into your system.
There are a variety of ways to assess how your implementation project is progressing,
some include:
- Chart audits to evaluate any of the process measures above:
- Can be conducted in real time or retrospectively.
- Can be all charts or some charts selected for surveillance using a sampling such as a random sample or systematic approach (e.g., every 5th pediatric patient over 10 years old), or all pediatric patients evaluated over a given time period.
- Survey staff on usage and/or comfort.
- Consider adding “survey staff experience/satisfaction” as a layer related to the implementation of any of your intervention strategies.
- Create a brief survey for families for any of the process measures above:
Some example numerical metrics you can calculate for each process measure are listed in the table below:

Below you will find suggested possible interventions, also called change strategies, for the process measure. These are suggestions on different steps that may assist your team in accomplishing the aim you are focusing on. Interventions or change strategies are often grouped into “Guidelines/Protocols, Education, Electronic Medical Records Optimization, and Resources (inclusive of personnel and equipment)”. As the local expert, you may have other ideas regarding how to best implement change in your hospital or ED. You should always feel free to reach out to your team leader and/or brainstorm these ideas with the other ED team leaders or participants working on similar aims in this collaborative.
Quality Measure: Percentage of pediatric patients with their weight documented only in kilograms
Policy statement
- Sites should define age range for pediatric population
- Weight should be recorded at every ED encounter
- Ensure that either an actual weight (i.e., gurney weight) or weight based on patient length (i.e., using the length-based tape) is used for all resuscitations
- Frequency that ED pharmacists attend a pediatric resuscitation and assist with medication administration
Infrastructure changes
- Utilize a scale that only weighs pediatric patients in kilograms or can be locked in kilograms mode
- Utilize gurney weights on all patients for whom staff are unable to get a scale weight
- Utilize a length-based tape and ensure that it is available/secured in resuscitation bay as well
- Utilize a single formulation for each medication
Electronic medical record (EMR) optimization
- EMR alerts care team when weight is not recorded in correct unit
- EMR alerts care team that weight does not coincide with patient’s height and age
- For resuscitation, weight is a required entry in the patient’s medical record
- Consider using standard weight nomograms (e.g., World Health Organization)
- EMR automatically calculates medication dosing based on weight recorded in kilograms in medical record
Education
- Integrate ED pharmacists into the healthcare team
- Develop training/educational content for care team
- Learning objectives should include: proper use of length-based tape, necessity of weight measurement required in cases of resuscitation, safety issues (e.g., number of reported medication errors), methods of measuring weight, nomograms, family engagement, your site’s policy; PRQC change strategies)
- Identify training modality (e.g., online, in-person, staff-meetings, peer to peer, EMR alerts)
- Identify strategies to increase families’ engagement
- Weight should not be estimated but measured
Knowledge reinforcement for care team
- Posters in triage area
- Direct feedback to care team following chart audits
- Develop script for use by triage nurse
Prescribing Patterns (deep dive for outcome measure)
- Manually track the number of incidences when an incorrect dose of a medication was ordered for a patient based on their weight
- Track high risk conditions with common errors in prescribing and administration medication administration (deep dive for outcome measure)
- Integrate a tool that nurses can reference to ensure that medication dosing is appropriate (use standard nomograms as reference)
- Integrate a nurse-to-nurse cross-check to ensure that medication dosing is appropriate. If site has bandwidth to accommodate this effort, consider cross-check for high-risk patients/medications or cross-checks during off-peak hours in the ED.
- Work with pharmacy team to develop notification system in the event that a prescribed medication does not coincide with standard practice
Patient & Family Engagement
- Include a process where families who ask about their child’s weight in pounds could be handed a preprinted chart and their child’s weight in kilograms and corresponding pounds could be circled
- Include process where family are advised of medication and dose prior to administration
- Disseminate weight infographic/conversion chart to empower caregiver engagement
Disclaimer: The views and responses to these FAQ’s are recommendations from the subject matter experts who presented during the Suicide Fireside Chat on August 8, 2023. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS, or the U.S. Government
If you have any additional questions, please email collaboratives@emscimprovement.center.
References
- American Academy of Pediatrics, Committee on Pediatric Emergency Medicine, American College of Emergency Physicians, Pediatric Committee, Emergency Nurses Association Pediatric Committee. Joint Policy Statement: Guidelines for care of children in emergency departments. Pediatrics 2009;124:1233-1243. doi: 10.1542/peds.2009-1807.
- American Academy of Pediatrics, Committee on Pediatric Emergency Medicine, American College of Emergency Physicians, Pediatric Committee, Emergency Nurses Association Pediatric Committee. Joint Policy Statement: Guidelines for care of children in emergency departments. Ann Emerg Med 2009; 54:543-52. doi:10.1016/j.annemergmed.2009.08.010.
- Remick K, Gausche-Hill M, Joseph M, Brown K, Snow S, Wright J. Pediatric readiness in the emergency department. Pediatrics 2018;142(5). doi: 10.1016/j.annemergmed.2009.08.010.
- Remick K, Gausche-Hill M, Joseph M, Brown K, Snow S, Wright J. Pediatric readiness in the emergency department. Ann Emerg Med 2018;72(6):e123-e136. doi: 10.1016/j.annemergmed.2018.08.431. [Epub ahead of print 2018 Nov 1]]
- Remick K, Gausche-Hill M, Joseph M, Brown K, Snow S, Wright J. Pediatric readiness in the emergency department. J Emerg Nurs 2019;45(1):e3-e18. doi: 10.1016/j.jen.2018.10.003. [Epub ahead of print 2018 Nov 1].
- Gausche Hill M, Ely M, Schmuhl P, Telford R, Remick K, Edgerton E, Olson L. National Assessment of Pediatric Readiness of Emergency Departments. JAMA Pediatrics. 2015 Jun; 169(6): 527-34. doi: 10.1001/jamapediatrics.2015.138.
- Remick KE, Hewes HA, Ely M, et al. National Assessment of Pediatric Readiness of US Emergency Departments During the COVID-19 Pandemic. JAMA Netw Open. Jul 3 2023;6(7):e2321707. doi:10.1001/jamanetworkopen.2023.21707
- Ames SG, Davis BS, Marin JR, Fink EL, Olson LM, Gausche-Hill M, Kahn JM. Effect of emergency department pediatric readiness on outcomes in critically ill children. Pediatrics 2019 144(3). e20190568. doi: 10.1542/peds.2019-0568.
- Newgard CD, Lin A, Olson LM, Cook JNB, Gausche-Hill M, Kuppermann N, Goldhaber-Fiebert JD, Malveau S, Smith M, Dai M, Nathens AB, Glass NE, Jenkins PC, McConnell KJ, Remick KE, Hewes H, Mann NC, Pediatric Readiness Study Group . Evaluation of emergency department Pediatric Readiness and outcomes among US Trauma Centers. JAMA Pediatr. 2021;175(9):947-956. doi: 10.1001/jamapediatrics.2021.1319.
- Newgard CD, Lin A, Malveau S, Cook JNB, Smith M, Kuppermann N, Remick KE, Gausche-Hill M, Goldhaber-Fiebert J, Burd RS, Hewes HA, Salvi A, Xin H, Ames SG, Jenkins PC, Marin J, Hansen M, Glass NE, Nathens AB, McConnell KJ, Dai M, Carr B, Ford R, Yanez D, Babcock SR, Lang B, Mann NC; Pediatric Readiness Study Group. Emergency department pediatric readiness and short-term and long-term mortality among children receiving emergency care. JAMA Netw Open. 2023 Jan 3;6(1):e2250941. doi: 10.1001/jamanetworkopen.2022.50941.PMID: 36637819.
- 11. Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press; 2000.
- American Academy of Pediatrics, National Initiative for Children’s Health Care Quality Project Advisory Committee. Principles of patient safety in pediatrics. Pediatrics. 2001;107(6):1473–1475
- American Academy of Pediatrics, Committee on Drugs and Committee on Hospital Care. Prevention of medication errors in the pediatric inpatient setting. Pediatrics. 2003;112(2):431– 436
- Steering Committee on Quality Improvement and Management and Committee on hospital Care. Policy Statement—Principles of Pediatric Patient Safety: Reducing Harm Due to Medical Care. Pediatrics 2011;127:1199–1210